In the excellent introductory feature to The Guardian’s week-long series on chronic pain and long Covid, Linda Geddes detailed the growing prevalence of chronic pain and the acceptance of nociplastic pain in the medical community.
Traditionally, doctors have divided pain into two categories: nociceptive pain, triggered by injuries such as bruises, burns, fractures, sprains or inflammatory conditions such as arthritis, and detected by pain receptors in our skin, bones and other tissues; and neuropathic pain triggered by damage to the nerves that carry sensory signals from these tissues to the brain and spinal cord.
But a few years ago, the IASP introduced a third category: nociplastic pain – pain arising from the altered processing of these sensory signals, without any evidence of actual or threatened tissue damage. One thing that can happen is that the pain signals carried by peripheral nerves from the skin, muscles, joints or internal organs to the spinal cord can become amplified, worsening the pain.
One expert likened it to “an allergic reaction in the pain system”.
Geddes says central sensitisation of the nervous system has been accepted by pain specialists, but it will take a while for it to flow into the wider medical community. As such, many patients’ experiences are dismissed by family doctors as being just in their heads because there are no obvious biomarkers of nociplastic pain. In many cases, their pain is treated with opioid drugs.
Although opioids are effective at dampening short-term severe pain or cancer pain, they are highly addictive and accidental overdose kills about 50,000 people in the US alone each year. They can also make chronic pain worse. This is because opioids provide relief by blocking pain receptors but your body responds by increasing the number of pain receptors, meaning you need higher doses to get the same relief. In chronic pain conditions such as fibromyalgia, people have already been producing natural opioids called endorphins, which bind to the same receptors. “Giving them an opioid is like throwing kerosene on to a fire,†says Daniel Clauw, a professor of anesthesiology, medicine and psychiatry at the University of Michigan.
Health authorities around the world are increasingly recommending non-pharmaceutical treatments for chronic pain and associated conditions.
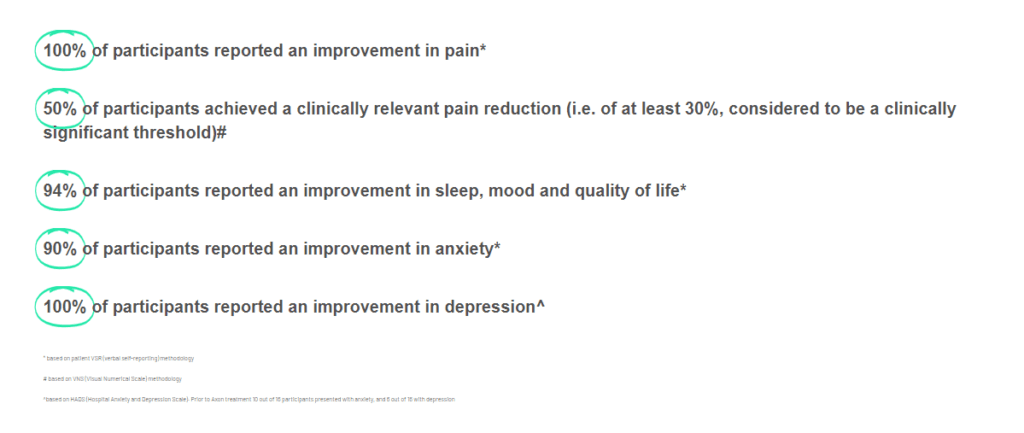
Exsurgo’s recent proof-of-concept trial in the UK showed that patients using the proprietary, non-pharmaceutical Axon system reported significant reductions in their levels of pain, anxiety and depression. At the same time, they reported improvements in sleep, mood and quality of life. Read more about the results here.